Research
National Nanotechnology Day: Rising to the challenges of COVID-19
October 09, 2020
National Nanotechnology Day is an annual event that celebrates nanotechnology and its impact on our world. The date, 10/9, pays homage to the nanometer scale: 10–9 meters.
The International Institute for Nanotechnology (IIN) is dedicated to nanoscience research that addresses the world’s most pressing problems. And in 2020, our world is facing a health crisis unlike any seen in more than a century: the COVID-19 pandemic. There has never been a greater need for interdisciplinary research that identifies critical needs in society and moves quickly to deliver solutions.
This year, for National Nanotechnology Day, we’re highlighting the ways that IIN-affiliated researchers have risen to the challenges of COVID-19. Many of these efforts began in the early days of the pandemic, and the stories below include updates on their progress to date, from groundbreaking improvements in personal protective equipment to research that targets the virus and points the way forward to valuable new therapeutics.
3D printers create face shield components for essential workers
 This spring, as the COVID-19 pandemic began to surge, there was a severe shortage of personal protective equipment (PPE) in hospitals. IIN Director Chad Mirkin and Northwestern graduates James Hedrick and David Walker from Azul 3D saw an opportunity to put a meaningful dent in that need by 3D printing face shields with the HARP (high-area rapid printing) technique developed at the IIN.
This spring, as the COVID-19 pandemic began to surge, there was a severe shortage of personal protective equipment (PPE) in hospitals. IIN Director Chad Mirkin and Northwestern graduates James Hedrick and David Walker from Azul 3D saw an opportunity to put a meaningful dent in that need by 3D printing face shields with the HARP (high-area rapid printing) technique developed at the IIN.
HARP uses projected ultraviolet light to cure liquid resins into hardened plastic. This process can print pieces that are hard, elastic, and mechanically robust, and they can be created at a record throughput for the field of 3D printing. For this effort, the HARP printers ran around the clock to produce PPE components, with volunteers working in six-hour shifts to keep the production cycle going continuously.
By the end of June, 3,886 face shields had been shipped to seven states in need. The majority were sent to the Navajo Nation, which has one of the highest rates of COVID-19. Materials have also gone to hospital COVID-19 wings and emergency rooms, first responders, nursing facilities, and other healthcare facilities.
Antiviral materials could deactivate virus upon contact
 In May, a team led by Omar Farha received a grant to develop antiviral textile materials for use in mask filters and face masks, with the goal of deactivating infectious viruses rather than merely slowing viral transmission.
In May, a team led by Omar Farha received a grant to develop antiviral textile materials for use in mask filters and face masks, with the goal of deactivating infectious viruses rather than merely slowing viral transmission.
Today, they are seeing encouraging preliminary results. Kaikai Ma, a postdoctoral researcher, immobilized active ingredients from commercially available disinfectants on textile materials. These fabrics inactivated both Gram-positive and Gram-negative bacteria within one minute. These promising results suggest the fabrics will display antiviral activity as well, which will soon be tested. Additionally, Ma is preparing a visible light-responsive mask by immobilizing a light-induced active species on the mask that will disinfect microbial species.
These active masks could serve as a valuable safeguard for civil and hospital use during COVID-19 and future pandemics.
UV-resistant elastic allows N95 masks to be safely reused
 In May, a team led by Mark Hersam received funding to develop a new elastic material that could enable N95 medical face masks to be disinfected and reused dozens of times.
In May, a team led by Mark Hersam received funding to develop a new elastic material that could enable N95 medical face masks to be disinfected and reused dozens of times.
The researchers have now successfully formulated graphene-based elastomeric composites that provide broad-spectrum ultraviolet resistance. They are currently integrating these materials into mask straps, so that N95 masks can be safely disinfected and reused following ultraviolet germicidal irradiation (UVGI).
This work has been accomplished by postdoctoral fellow Dr. Ana Carolina Mazarin de Moraes and PhD students Lidia Kuo and Shay Goff Wallace from the Hersam Group.
On-mask chemical modulation strategy shows results
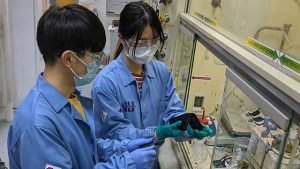 In March, Jiaxing Huang received funding to develop a mask-inspired structure that would help to make an infected person, either symptomatic or asymptomatic, less infectious. Huang’s team investigated anti-viral chemicals that could be safely built into masks and sanitize any escaped respiratory droplets, providing additional chemistry-based protection beyond a physical barrier.
In March, Jiaxing Huang received funding to develop a mask-inspired structure that would help to make an infected person, either symptomatic or asymptomatic, less infectious. Huang’s team investigated anti-viral chemicals that could be safely built into masks and sanitize any escaped respiratory droplets, providing additional chemistry-based protection beyond a physical barrier.
Their findings are about to be published in the journal Matter where they will report that their on-mask chemical modulation strategy can indeed contaminate the escaped respiratory droplets with a high dosage of anti-viral compounds during simulated sneezing and coughing, even when used with a layer of medical gauze with low fiber density that barely hinders breathing. This strategy could help reduce the sources of viral transmission and strengthen the public health response to control and mitigate the outbreak of infectious respiratory diseases.
The team includes Haiyue Huang, a Ryan Fellow, and Hun Park, a postdoctoral fellow. They are joined by Yihan Liu, an MS student who contributed data analysis and coding. Simona Fine, an undergraduate, is working on another mask concept using common fabrics based on “home experiments” they supervised remotely over the summer. Huang’s lab is also working on designing face shields that can hinder the release of respiratory aerosols and anti-viral coatings on stainless steel that can help to suppress fomite infections.
Quick-screen technology could enable rapid, easy-to-use tests for infectious diseases
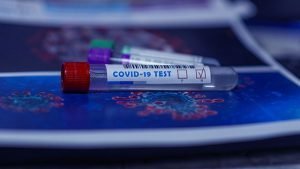 In April, a team of IIN-affiliated researchers led by Michael Jewett and Julius Lucks received funding to develop a quick-screen technology that can test for infectious diseases, including COVID-19, in the human body or within the environment.
In April, a team of IIN-affiliated researchers led by Michael Jewett and Julius Lucks received funding to develop a quick-screen technology that can test for infectious diseases, including COVID-19, in the human body or within the environment.
Similar to a pregnancy test, the tool uses one sample to provide an easy-to-read negative or positive result. By simplifying testing, the researchers could put diagnostics into the hands of people everywhere — without the need for expensive laboratories or expertise.
Today, Lucks reports that they have a promising assay working in the lab and are now transitioning to the next steps of optimization and testing. The core team of students working on the project includes Kirsten Jung, Matt Verosloff, Grant Rybnicky, Mara de Lourdes Cabezas, Joe Muldoon, and Walter Thavarajah.
Cell-free biotechnology could help accelerate COVID-19 therapeutics
 In April, researchers at Northwestern and Cornell Universities announced a new platform that could produce new therapies more than 10 times faster than current methods. After taking the molecular machinery out of bacteria, the researchers use that machinery to make a product, such as therapeutics, in a safe, inexpensive and rapid manner.
In April, researchers at Northwestern and Cornell Universities announced a new platform that could produce new therapies more than 10 times faster than current methods. After taking the molecular machinery out of bacteria, the researchers use that machinery to make a product, such as therapeutics, in a safe, inexpensive and rapid manner.
Led by Michael Jewett, the team had been using the synthetic biology-based platform to mass manufacture potential protein therapeutics for cancer. But they quickly pivoted to leverage the technology to help address the novel coronavirus pandemic. Through their startup company, SwiftScale Biologics, the researchers began working to mass produce a promising antibody therapy developed by an outside biotherapeutics company.
Since then, Swiftscale Biologics has continued to advance their novel cell-free protein synthesis technology to accelerate manufacturing and scale-up of COVID-19 neutralizing antivirals. Their technology reduces the time from DNA to clinical scale doses from the typical 18 months to 4-6 weeks. Swiftscale has teamed up with multiple commercial partners towards bringing new drugs to market faster. At this stage, several therapeutic antiviral proteins have shown the ability to protect hamsters from SARS-CoV-2, the COVID-19-causing coronavirus.
Nanometer-level simulations expose new vulnerability in SARS-CoV-2
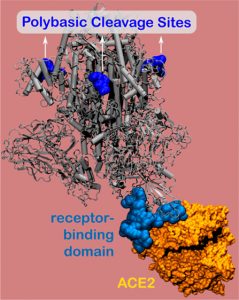 In August, IIN-affiliated researchers uncovered a new vulnerability in the novel coronavirus’ infamous spike protein — illuminating a relatively simple, potential treatment pathway.
In August, IIN-affiliated researchers uncovered a new vulnerability in the novel coronavirus’ infamous spike protein — illuminating a relatively simple, potential treatment pathway.
Using nanometer-level simulations, researchers led by Monica Olvera de la Cruz discovered a positively charged site located 10 nanometers from the actual binding site on the spike protein. The positively charged site allows strong bonding between the virus protein and the negatively charged human-cell receptors.
Leveraging this discovery, the researchers designed a negatively charged molecule that inhibits the virus from bonding to the host cell. Olvera de la Cruz and her team are now continuing this research with colleagues at Northwestern.
Nanostructured therapy targets the spike proteins of the coronavirus
 In April, researchers led by Samuel Stupp announced work on a new nanostructured therapy that could potentially disable the virus and prevent its infection of human cells. This new peptide-based therapeutic aims to target and disable the coronavirus’ so-called “spike proteins,” which attach to and infect healthy cells.
In April, researchers led by Samuel Stupp announced work on a new nanostructured therapy that could potentially disable the virus and prevent its infection of human cells. This new peptide-based therapeutic aims to target and disable the coronavirus’ so-called “spike proteins,” which attach to and infect healthy cells.
The researchers “glue” millions of peptides into a nanostructure that becomes the carrier of the precious drugs. The similar chemistry of the drug and the carrier allows the researchers to design nanostructures that protect the peptide drug while it circulates in the body before it encounters the culprit of the disease, the novel coronavirus. The core team working on this project includes Mark Karver and Suvendu Biswas of the Simpson Querrey Institute, along with Tristan Clemons and Ruomeng Qiu from the Stupp Laboratory.
Projects like this show the importance of collaborative interdisciplinary research, which is at the heart of nanotechnology at Northwestern.
“When there’s a crisis, you never know what areas of science will be needed to address a specific challenge,” Stupp says. “You have to draw from many parts of science to solve problems, and it’s very difficult to predict which ones will be the most useful. This pandemic illustrates a very important point: that even though I was not focused on viral infections, I was able to use my knowledge and my experience in something else that is directly applicable to the current COVID-19 challenge.”